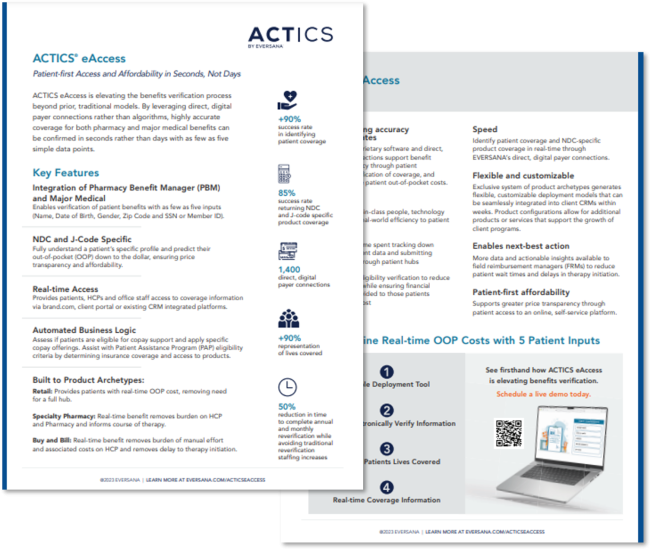
Patient-first Access and Affordability Through Electronic Benefits Verification and Prior Authorization Submissions
Current electronic benefits verification (eBV) and electronic prior authorization (ePA) tools fail to meet the needs of patients. In many cases only 60% of the electronic verification results are accurate and more than 70% of prior authorization submissions are rejected with little to no reporting on the patient’s status. ACTICS eAccess, EVERSANA’s new proprietary eBV and ePA platform, improves patient access and accelerates speed to therapy.
Elevating the Benefits Verification Process
Verifying a patient’s insurance eligibility should be a simple and straightforward process. Unfortunately, it is most often a painstaking process that consumes HCP staffs’ time, causes confusion and frustration due to inaccurate information, and most significantly, delays initiating treatment for patients in need.
EVERSANA’s eBV tool is elevating the benefits verification process beyond prior, traditional models. By leveraging over 1,400 digital connections to payers rather than algorithms, highly accurate coverage for both pharmacy and major medical benefits can be confirmed in minutes rather than days – with as few as five simple data points.