
Rich Heddens
SVP, Payer Strategy & Execution
Expertise:
Rich Heddens, Senior Vice President of Payer Strategy & Execution, is helping EVERSANA’s partners drive life-changing therapies to market and into the hands of patients. As a leader in market access, sales and marketing for pharma and biotech, Rich has 20 years of experience in business development and client management. Through his career at companies, such as MedImmune, Novartis, inVentiv Health and Syneos Health, he specializes in managed markets, field sales, account management and national account management, reimbursement practices, market access and public health. He las led more than 20 pharma and biopharma product launches across multiple disease and treatment areas.
Rich earned his bachelor’s degree in business from the University of Wisconsin – La Crosse.
Articles by Rich Heddens
Payer Oncology Access Management in 2022
Payers balance the severity of disease with the need to control high-dollar utilization. As pharmacy spend continues to rise, payers are seeking ways to manage costs in the highest cost therapeutic areas, including oncology. While there is appetite to manage access for both oral and office-administered oncology agents, payers struggle with which tactics to implement without sacrificing patient outcomes. Pharmaceutical companies should expect to see changes in payer management for oncology over the next 2-3 years. In a recent article, the NAVLIN Insights team outlines payer access management in oncology today and takes a closer look at how access will evolve in the coming years, including the impact of the Inflation Reduction Act and which brands may […]

Accelerate Patient Therapy Adoption by Eliminating Obstructive Pain Points and Waiting Games
Acquiring all the necessary information to initiate patients’ treatment can sometimes feel like a bad game of Telephone to HCPs and their staff. Missing or inaccurate details that can require multiple phone calls, emails or faxes to various individuals can eat up staffs’ time and resources and prolong patients’ adoption of therapy. EVERSANA’s Field Reimbursement Managers (FRMs) work in conjunction with patient services teams through established relationships and a secure integrated messaging portal. HCP offices can lean on one contact for the information they need and access it directly in front of them using our interconnected communication channels. Our FRMs know what is necessary for prior authorization approvals and work with […]

Elevate Your Brand to New Heights by Utilizing National Account Managers’ Singular Skills, Resources and Experience in an Ever-changing Marketplace
Launching new therapies is a vast undertaking for any pharmaceutical company. Setting up a product for success requires a great deal of expense, research, strategic planning and effective collaboration, just to name a few essential elements. EVERSANA’s National Account Managers (NAMs) serve as fully integrated partners to manufacturers, invested in the success of their products and in creating ample accessibility for patients who will benefit from them. Our NAMs support our partners’ new and existing brands by utilizing our unique experience and resources to bring stability and sustainability to their products prior to, during and after launch. While today’s NAMs face unprecedented challenges – specifically in a post-pandemic market – EVERSANA knows how to address those […]

Connectivity Between Field Reimbursement Managers and Patient Services: The Missing Link to Efficiency
EVERSANA’s Rich Heddens, Senior Vice President, Payer Strategy & Execution, and Matthew Baniak, Vice President, Client Delivery & Excellence, discuss the importance of connectivity between Field Reimbursement Managers (FRMs) and Patient Services. Disparate information, antiquated systems and a disconnect between the two service areas often translate to pain points experienced by patients and providers. EVERSANA’s three pillars, people, data and infrastructure, bridge the gap to create efficient and effective communications, ultimately reducing frustrations and getting the patient on therapy faster. In this video, the two industry leaders cover: Why the connectivity of Field Reimbursement Managers and the Patient Services team is important to ensure patients’ adoption of new therapies How […]

Innovative Payer Strategies Demand Innovative NAM Strategies
EVERSANA’s Rich Heddens, Senior Vice President, Payer Strategy & Execution, and Dino Tsamparlis, Vice President, Market Access, discuss how innovative payer strategies call for innovative National Account Manager (NAM) strategies. The industry is facing unique challenges that did not exist prior to COVID-19. Payer mixes have changed substantially in the U.S., subsequently altering the economics in the payers’ minds prompting them to think more deeply about their strategies, their modeling and how they treat products. In addition, the big players continue to consolidate, lending fewer controllers over the plans influencing the U.S. Lastly, complex therapies continue to dominate the market. EVERSANA is uniquely positioned to address current industry challenges […]
EVERSANA’s Integrated Operations, Data-Driven Solutions and Digital Expertise Solve Key Challenges in Market Access and Field Deployment
Pharmaceutical manufacturers relying on the standard model for executing market access and field deployment strategies utilize resources inefficiently and redundantly. By integrating actions across operations, manufacturers can right size company resources, ensure affordability and increase speed to therapy. Four key industry-wide challenges have been identified in market access and field deployment. EVERSANA’s next generation model featuring integrated operations, data-driven solutions and digital expertise can directly address these trends and optimize frontline strategies. Challenge: The pharmaceutical industry recently pivoted to a virtual field model; however, in-person HCP-Rep engagement is still relevant, especially for promotionally sensitive brands and complex disease states. Manufacturers must now adapt to HCPs’ communication preferences and balance hybrid […]

Informing NAMs Payer Strategies and Improving Contracts With Integrated Commercial Services
Pharmaceutical manufacturers rely on national account managers (NAMs) to build relationships, negotiate contracts and get their products in front of payers and pharmacy benefit managers who will clear the way for patient treatment coverage. Challenges Facing NAMs Typically, NAMs rely on the customer or the health plan to direct contracting strategies and product expectations, and they often manage contracts in a silo without input from other commercial services teams. While NAMs may have some data insights, the disconnect between commercial services causes them to inefficiently leverage data or miss insights that could lead to optimized contracting strategies. Without data integration, NAMs cannot pinpoint the patient populations and treatment indicators for […]
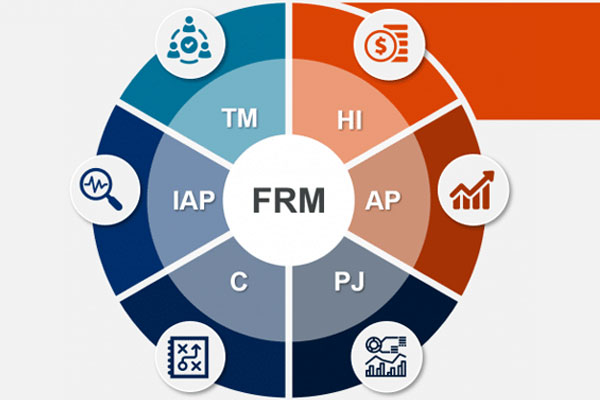
Revolutionizing FRMs With Data Connectivity and Commercial Services Integration
FRMs, sometimes referred to as field reimbursement specialists or patient experience specialists, are the key drivers in patient pre-authorization and billing and coding processes, and play a vital role in the prescription and adoption of specialty drugs. While field reps focus on selling, FRMs focus solely on supporting healthcare provider (HCP) offices and helping office staff get past complex processes and procedures that can hinder speed-to-therapy for patients. Challenges Facing FRMs The highly technical nature of the FRM role is already challenging and becomes further complicated by a lack of connectivity and process inefficiency with hub and data and analytics teams. Manufacturers and life sciences companies realize that connectivity for […]

